59 yr old male
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs. This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box.
Came with chief complaints of fever since one day associated with chills and rigour
Also was suffering with loose stools since yesterday ( several episodes of liquid consistency stools) and 5 episodes of vomiting since yesterday.
HOPI
Patient was apparently asymptomatic 1day ago then he developed high grade fever which was associated with chills and rigours followed by several episodes of loose stools which were not blood stained and not foul smelling.he also had 5 episodes of vomiting since yesterday.
Not a known case of HTN,CAD,TB,ASTHMA AND EPILEPSY
(Had history of DM 3 years back and used METFORMIN for 3 months)
on admission
Patient is conscious coherent cooperative
BP: 100/70mmhg
PR:112
Temp:101f
CVS:S1 S2+
RS: BAE+
CNS: NAD
P/A:soft,non tender
No pallor, icterus, cyanosis, clubbing, and lymphadenopathy
Appetite:normal
Diet:mixed
Bowel and bladder:regular
Sleep: adequate
No significant family history
In each episode, the stools produced are yellow in colour ,large volume and of watery consistency
Previous history: he presented with similar complaints in the past at this hospital
And was treated with
Tab. Pan 40 mg od for 7 days
Tab. METFORMIN 500 mg for 7 days
Tab.bescoules od for 7 days
Inj. Ciprofloxacin 500 mg IV BD for 5 days
Inj. Metrogyl 500 mg IV tid for 5 days
Inj. Optineruron 1 amp in 1ns iv OD
Tab. Sporlac -ds tid
Ors sachet in 1lit. Water
Grbs before breakfast, 2hrs after lunch and 2hrs after dinner.
He was also discovered to be HIV positive in this hospital.
there was no history blood transfusion in the past, and no history of needle prick.
Provisional diagnosis: acute gastroenteritis
Investigations
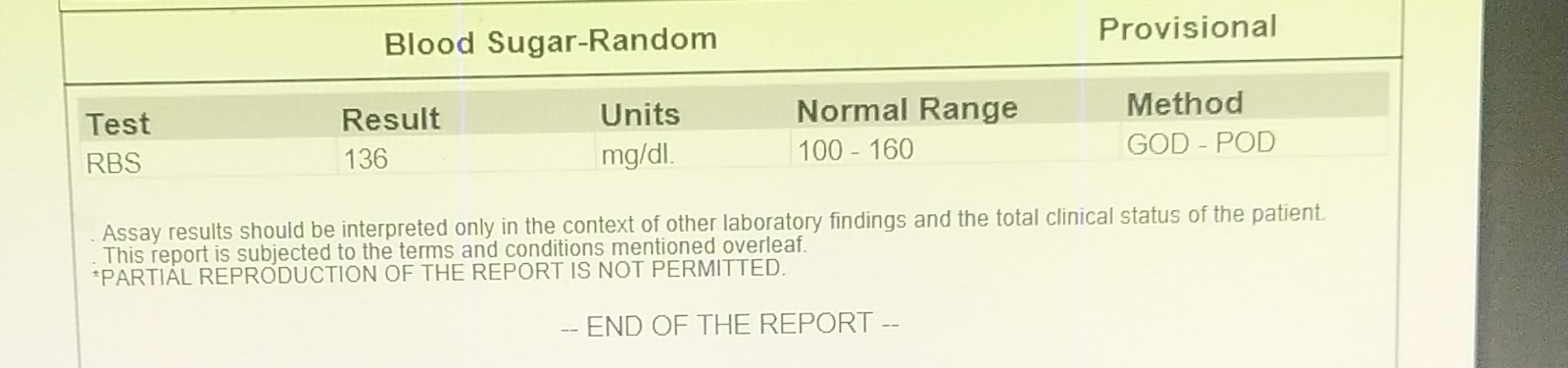
RBS
LFT
RFT
Cue
Hemogram
Anti hcv ab
Fever chart
Stool report
Treatment:
Inj. Neomol 1gm, if stat (if temp more than 101f)
Tab. Sportscaster DS PO TID
Tab pan 40MG PO OD
IV FLUIDS NS @50 ml/hr
Tab dolo 650 mpg
GRBS monitoring 6th hourly
BP, PR monitoring 12th hourly
temp monitoring 4th hourly PO TID
Found to be HIV positive in this hospital
So started on ART.
Discharge summary


























Comments
Post a Comment