FINAL EXAMINATION CASE REPORT
NAME: Harsha ch.
Hall ticket no: 1701006029
Batch: 2017
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs. This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box"
abdominal distension - insidious in onset, gradually progressive to the present size - associated with
- Pain in epigastric and right hypocondrium - colicky type.
- Fever - high grade, not associated with chills and rigor, decreased on medication, No night sweats.
- Not associated with Nausea, vomiting, loose stools
There was pedal edema
- Gradually progressive
- Pitting type
- Bilateral
- Below knees
- Increases during the day - maximum at evening.
- No local rise of temperature and tenderness
- Grade 2
- Not relived on rest
He also complained of shortness of breath - grade 4
- Insidious in onset
- Gradually progressive
- Agrevated on eating and lying down ; No relieving factors
- No PND
- No cough/sputum/hemoptysis
- No chest pain
- No wheezing
Patient is a known alcoholic since 20 years. Had his last drink on 29th May, 2022.
Daily Routine :
Wakes up at 5am and goes to field.
Comes home at 8am and has rice for breakfast. Returns to work at 9am.
1pm - lunch
2-6 pm - work
6pm - home
8pm - dinner
Daily Drinks after field work
PAST HISTORY:
No history of similar complaints in the past
Medical history- not a known case of DM, HTN, TB, Epilepsy, Asthma, CAD
Surgical history - not significant
PERSONAL HISTORY:
- Diet - mixed
- Appetite- reduced since 7 days
- Sleep - disturbed
- Bowel - regular
- Bladder - oliguria since 2 days, no burning micturition, feeling of incomplete voiding.
- Allergies- none
- Addictions - Beedi - 8-10/day since 20 years ;
- Alcohol - Toddy - 1 bottle, daily, since 20 years;
- Whiskey-180 ml, 2 times a week, since 5 years,
But stopped 6 months back
- Last alcohol intake - 29th May, 2022. ( Sunday)( beer and toddy)
-FAMILY HISTORY:
Not significant
GENERAL EXAMINATION:
Patient is conscious, coherent and co-operative.
Examined in a well lit room.
Moderately built and nourished
Icterus - present (sclera)
Pedal edema - present - bilateral pitting type, grade 2
No pallor, cyanosis, clubbing, lymphoedenopathy.
Vitals :
Temperature- febrile
Respiratory rate - 16cpm
Pulse rate - 101 bpm
BP - 120/80 mm Hg.
SYSTEMIC EXAMINATION:
CVS : S1 S2 heard, no murmurs
Respiratory system : normal vesicular breath sounds heard.
Abdominal examination:
INSPECTION :
Shape of abdomen- distended
- Umblicus - everted
- Movements of abdominal wall - moves with respiration
- Skin is smooth and shiny;
- No scars, sinuses, distended veins, striae.
PALPATION :
Local rise of temperature present.
Tenderness present - epigastrium.
Tense abdomen
Guarding present
Rigidity absent
Fluid thrill positive
Liver not palpable
Spleen not palpable
Kidneys not palpable
Lymph nodes not palpable
PERCUSSION:
Liver span : not detectable
Fluid thrill: felt
AUSCULTATION:
Bowel sounds: heard in the right iliac region
CNS EXAMINATION:
Conscious
Speech normal
No signs of meningeal irritation
Cranial nerves: normal
Sensory system: normal
Motor system: normal
Reflexes: Right. Left.
Biceps. ++. ++
Triceps. ++. ++
Supinator ++. ++
Knee. ++. ++
Ankle ++. ++
Gait: normal
INVESTIGATIONS:
Serology:
HIV - negative
HCV - negative
HBsAg - negative
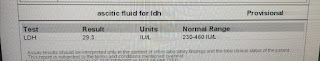
Ascitic tap
PROVISIONAL DIAGNOSIS:
Acute decompensated liver failure with ascites.
TREATMENT:
Syp. Lactose 15ml TID
Abdominal girth charting - 4th hourly
Fluid restrictriction less than 1L per day
Salt restriction less than 2 gms per day


































Comments
Post a Comment